
As we age, our vulnerability to certain health issues, like kidney disease, increases. This condition, common among the elderly, can silently progress if not detected early. In this article, will explore kidney disease's impact on the senior population, stressing the importance of awareness and timely intervention.
Understanding Kidney Disease
These bean-shaped organs serve as our body’s sophisticated filtration system, ensuring that our body remains in equilibrium.
The Role of Kidneys
Our kidneys tirelessly filter large volumes of blood daily, removing waste products and excess water. This waste and excess water become urine, which the kidneys send to the bladder for excretion.
Beyond filtration, kidneys regulate essential bodily functions. They maintain the balance of electrolytes, like sodium, potassium, and calcium. They also produce hormones that regulate blood pressure, create red blood cells, and keep bones healthy.
What Is Kidney Disease?
Kidney disease can be either chronic or acute. Acute kidney disease is often temporary and can be caused by a sudden injury or trauma, while chronic kidney disease (CKD) develops over time and is usually permanent.
CKD means your kidneys are damaged and can't filter blood the way they should. This damage can cause wastes to build up in the body, leading to further health complications. CKD often progresses stealthily, with symptoms becoming apparent only in the later stages.
Stages and Progression
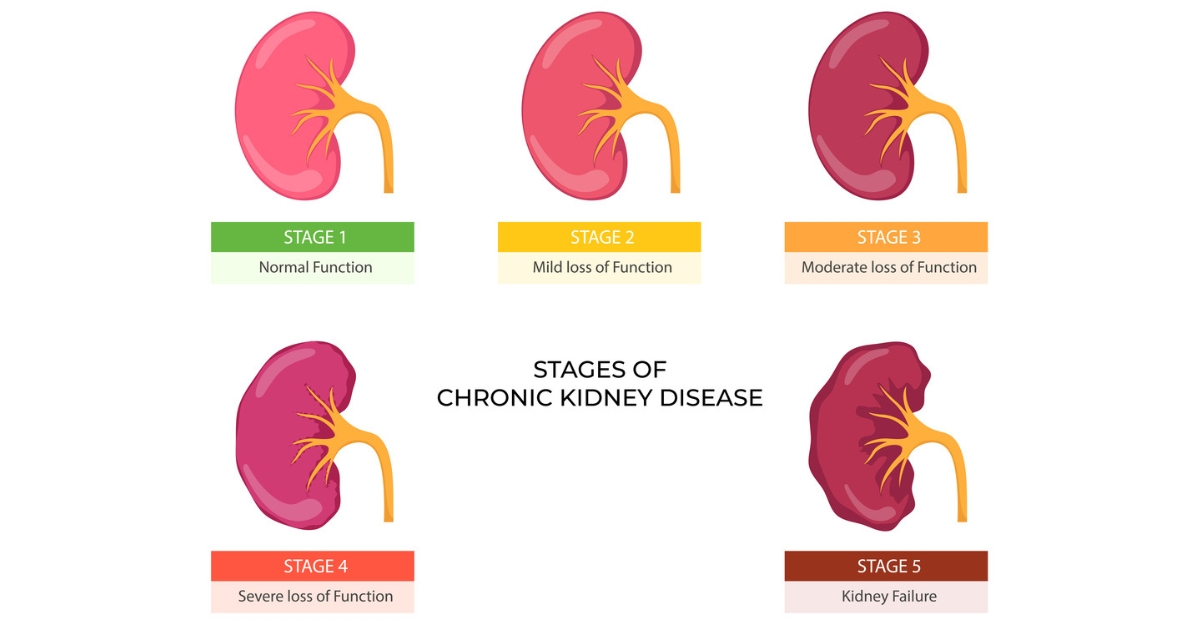
CKD is categorized into five stages, with the fifth stage being the most severe. These stages are determined based on the kidneys' filtering capabilities, known as the Glomerular Filtration Rate (GFR). As chronic kidney disease progresses, the GFR decreases.
Early-stage CKD may not have noticeable symptoms. But as the disease advances, symptoms like swelling, fatigue, difficulty concentrating, and decreased appetite can manifest.
Impact on the Elderly
The body's natural aging process can make the elderly more susceptible to CKD and its complications, including kidney failure. As we age, kidney function gradually decreases, making any additional injury or disease more impactful.
Moreover, other age-associated conditions like diabetes, high blood pressure, or heart disease can further contribute to kidney deterioration in the elderly.
Causes and Risk Factors
Primary Causes of Kidney Disease in the Elderly
- Diabetes: High blood sugar can, over time, damage the tiny blood vessels in the kidneys. This can impair their ability to filter waste, making diabetes one of the leading causes of kidney disease.
- High Blood Pressure (Hypertension): Just as it can harm blood vessels in other parts of the body, persistent high blood pressure can also damage the kidney's blood vessels, reducing their filtration capacity.
- Glomerulonephritis: An inflammation of the kidney's filtering units, this can sometimes result from an infection or other triggers. Though it can be treated, it might lead to kidney damage over time.
- Polycystic Kidney Disease: A genetic disorder characterized by the growth of numerous cysts in the kidneys, potentially impairing kidney function.
Medications and Treatment Side Effects
Some medications, especially when consumed in large quantities or over extended periods, can have nephrotoxic effects. Over-the-counter painkillers like ibuprofen or certain prescription drugs might increase the risk of kidney damage.
Lifestyle and Environmental Factors
- Chronic Urinary Tract Infections: Recurrent UTIs can sometimes cause scarring, which might affect the kidneys.
- Exposure to Toxins: Prolonged exposure to certain chemicals or toxins can pose risks to kidney health. This includes some industrial chemicals or certain medications.
Other Risk Factors
- Cardiovascular Disease: A history of heart disease or stroke can increase the risk of kidney disease.
- Obesity: Being significantly overweight can raise the risk of developing diabetes and high blood pressure, two major risk factors for developing kidney disease.
- Age: The process of aging can make the kidneys more vulnerable to various diseases and conditions.
- Family History: Genetics can play a role. A family history of kidney disease can increase an individual's risk.
Symptoms and Diagnosis
Especially for our elderly loved ones, recognizing these signs can be the difference between early intervention and more advanced complications. Beyond just clinical indicators, understanding symptoms is about preserving moments of joy, unhindered by health issues.
Let's explore the symptoms of kidney disease and the steps to diagnose it.
Symptoms
- General Fatigue: One of the kidneys' roles is to produce a hormone (erythropoietin) that aids in red blood cell production. Reduced kidney function can lead to fewer red blood cells, causing fatigue and weakness.
- Fluid Retention: Swelling in the legs, ankles, feet, or even puffiness around the eyes can indicate the kidneys' inability to expel excess fluid.
- Urinary Changes: This can include frequent urination, especially at night, blood in the urine, foamy urine, or even difficulty in urinating.
- Skin Ailments: Itchy skin or darkening can arise due to the buildup of waste products in the bloodstream.
- Appetite Loss and Nausea: A build-up of toxins can affect taste, leading to decreased appetite and consistent feelings of nausea.
- Shortness of Breath: Fluid build-up in the lungs and anemia associated with kidney disease can cause breathlessness.
- Cold Sensitivity: Anemia can also lead to feeling cold even when in a warm environment.
Diagnosis and Screening
- Blood Tests: One of the primary diagnostic tools is the serum creatinine test, which measures the amount of waste in the blood. The result is then used to estimate the Glomerular Filtration Rate (GFR), which indicates kidney function levels.
- Urine Tests: These can detect abnormalities like protein or blood in the urine, which can be early indicators of kidney disease.
- Ultrasound: An imaging test that provides a visual of the kidneys, helping doctors spot any physical abnormalities or blockages.
- Kidney Biopsy: In cases where the cause of the symptoms is uncertain, a small sample of kidney tissue may be extracted for examination.
- Regular Screenings: For the elderly, especially those with risk factors like diabetes or hypertension, regular kidney function screenings are essential. Early detection can vastly improve outcomes and treatment options.

Management and Treatment
Kidney disease, particularly when identified in its early stages, can often be managed effectively, helping to slow its progression and mitigate its effects. For the elderly, a combination of medical treatments and lifestyle modifications plays a crucial role.
Here's a breakdown of the management and treatment options for kidney disease in older adults:
Lifestyle Changes
- Dietary Adjustments: Consuming a kidney-friendly diet is essential. This often means moderating protein intake, reducing salt, and avoiding foods high in potassium and phosphorus. A renal dietitian can provide personalized advice tailored to the individual's needs.
- Hydration: While it's essential to stay hydrated, those with kidney disease may need to monitor their fluid intake, especially if there are signs of fluid retention.
- Exercise: Engaging in regular, moderate exercise can help maintain kidney function, promote a healthy weight, and overall health. However, always consult a doctor before starting any exercise regimen.
Medications
- Blood Pressure Control: Hypertension can accelerate kidney damage. Medications like ACE inhibitors or ARBs can help control blood pressure and simultaneously reduce strain on the kidneys.
- Blood Sugar Management: For diabetics, controlling blood sugar levels is vital to prevent further kidney damage. Insulin and oral hypoglycemic agents are commonly prescribed.
- Cholesterol Control: Medications such as statins might be prescribed to manage cholesterol levels, thereby reducing cardiovascular complications associated with kidney disease.
- Anemia Treatment: Erythropoiesis-stimulating agents (ESAs) and iron supplements can help address anemia often seen in CKD patients.
- Mineral and Bone Disorder Management: Medications that help control phosphorus, calcium, and parathyroid hormone levels can prevent bone disease and other complications.
Dialysis
- Hemodialysis: This process involves filtering the blood outside the body through a machine. Typically, hemodialysis is done three times a week at a dialysis center.
- Peritoneal Dialysis: This can often be done at home. It involves inserting a cleaning solution into the abdomen, which absorbs waste products and is then drained out.
Kidney Transplant
While not always an option for the elderly due to other health conditions or the scarcity of donor kidneys, a transplant can provide a higher quality of life than dialysis. The feasibility of a transplant largely depends on the individual's overall health.
Regular Monitoring
Given the progressive nature of kidney disease, regular check-ups are vital. These appointments will monitor kidney function, adjust medications, and ensure no complications are developing.

Reclaiming Kidney Health
While the onset and progression of kidney disease can be daunting, armed with the right knowledge and resources, both patients and caregivers can navigate this journey with greater confidence.
By emphasizing the importance of regular medical check-ups, tailored treatments, and a kidney-friendly lifestyle, we can make significant strides in improving the quality of life for our senior loved ones.
If your elderly loved ones are dealing with kidney disease or other degenerative conditions, Keystone Health offers specialized house call providers skilled in managing complex medical needs. From dementia care to cardiology and cancer care, let Keystone be your trusted partner, ensuring quality, compassion, and expertise at every step.
